Achalasia
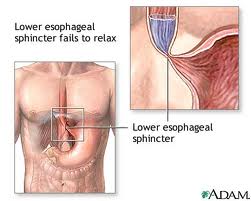
Achalasia is a rare disease of the muscle of the esophagus (swallowing tube). The term achalasia means "failure to relax" and refers to the inability of the lower esophageal sphincter (a ring of muscle situated between the lower esophagus and the stomach) to open and let food pass into the stomach. As a result, patients with achalasia have difficulty in swallowing food.
Causes
The cause of achalasia is unknown. Theories on causation invoke infection, heredity or an abnormality of the immune system that causes the body itself to damage the esophagus (autoimmune disease).
The esophagus contains both muscles and nerves. The nerves coordinate the relaxation and opening of the sphincters as well as the peristaltic waves in the body of the esophagus. Achalasia has effects on both the muscles and nerves of the esophagus; however, the effects on the nerves are believed to be the most important. Early in achalasia, inflammation can be seen (when examined under the microscope) in the muscle of the lower esophagus, especially around the nerves. As the disease progresses, the nerves begin to degenerate and ultimately disappear, particularly the nerves that cause the lower esophageal sphincter to relax. Still later in the progression of the disease, muscle cells begin to degenerate, possibly because of the damage to the nerves. The result of these changes is a lower sphincter that cannot relax and muscle in the lower esophageal body that cannot support peristaltic waves. With time, the body of the esophagus stretches and becomes enlarged (dilated).
Symptoms
The most common symptom of achalasia is difficulty in swallowing (dysphagia). Patients typically describe food sticking in the chest after it is swallowed. Dysphagia occurs with both solid and liquid food. Moreover, the dysphagia is consistent, meaning that it occurs during virtually every meal.
Sometimes, patients will describe a heavy sensation in their chest after eating that may force them to stop eating. Occasionally, pain may be severe and mimic heart pain (angina). The cause of this discomfort is felt to be the accumulation of ingested food within the esophagus.
Regurgitation of food that is trapped in the esophagus can occur, especially when the esophagus is dilated. If the regurgitation happens at night while the patient is sleeping, food can enter the throat and cause coughing and choking. If the food enters the trachea (windpipe) and lung, it can lead to infection (aspiration pneumonia).
Because of the problem with swallowing food, a large proportion of patients with achalasia lose weight. Episodes of chest pain may also occur especially with vigorous achalasia. Sometimes symptoms suggest gastroesophageal reflux disease (GERD); however, it's not clear if the symptoms are, in fact, due to reflux. Moreover, acid suppression rarely improves the symptoms of achalasia.
Treatment
Treatments for achalasia include oral medications, stretching of the lower esophageal sphincter (dilation), surgery to cut the sphincter (esophagomyotomy), and the injection of botulinum toxin (Botox) into the sphincter. All four treatments reduce the pressure within the lower esophageal sphincter to allow easier passage of food from the esophagus into the stomach.
Oral medications
Oral medications that help to relax the lower esophageal sphincter include groups of drugs called nitrates, for example, isosorbide dinitrate (Isordil) and calcium channel blockers, for example, nifedipine (Procardia) and verapamil (Calan). Although some patients with achalasia, particularly early in the disease, have improvement of symptoms with medications, most do not. By themselves, oral medications are likely to provide only short-term and not long-term relief of the symptoms of achalasia, and many patients experience side-effects from the medications.
Dilation
The lower esophageal sphincter also may be treated directly by forceful dilation. Dilation of the lower esophageal sphincter is done by having the patient swallow a tube with a balloon at the end. The balloon is placed across the lower sphincter with the help of X-rays, and the balloon is blown up suddenly. The goal is to stretch--actually to tear--the sphincter. The success of forceful dilation has been reported to be between 60% and 95%. Patients in whom dilation is not successful can undergo further dilations, but the rate of success decreases with each additional dilation. If dilation is not successful, the sphincter may still be treated surgically. The main complication of forceful dilation is rupture of the esophagus, which occurs 5% of the time. Half of the ruptures heal without surgery, though patients with rupture who do not require surgery should be followed closely and treated with antibiotics. The other half of ruptures require surgery. (Although surgery carries additional risk for the patient, surgery can repair the rupture as well as permanently treat the achalasia with esophagomyotomy.) Death following forceful dilation is rare. Dilation is a quick and inexpensive procedure compared with surgery, and requires only a short hospital stay.
Esophagomyotomy
The sphincter also can be cut surgically, a procedure called esophagomyotomy. The surgery can be done using an abdominal incision or laparoscopically through small punctures in the abdomen. In general, the laparoscopic approach is used with uncomplicated achalasia. Alternatively, the surgery can be done with a large incision or laparoscopically through the chest. Esophagomyotomy is more successful than forceful dilation, probably because the pressure in the lower sphincter is reduced to a greater extent and more reliably; 80%-90% of patients have good results. With prolonged follow-up, however, some patients develop recurrent dysphagia. Thus, esophagomyotomy does not guarantee a permanent cure. The most important side effect from the more reliable and greater reduction in pressure with esophagomyotomy, is reflux of acid (gastroesophageal reflux disease or GERD). In order to prevent this, the esophagomyotomy can be modified so that it doesn't completely cut the sphincter or the esophagomyotomy may be combined with anti-reflux surgery (fundoplication). Whichever surgical procedure is done, some physicians recommend life-long treatment with oral medications for acid reflux. Others recommend 24 hour esophageal acid testing with lifelong medication only if acid reflux is found.
Achalasia is a rare disease of the muscle of the esophagus (swallowing tube). The term achalasia means "failure to relax" and refers to the inability of the lower esophageal sphincter (a ring of muscle situated between the lower esophagus and the stomach) to open and let food pass into the stomach. As a result, patients with achalasia have difficulty in swallowing food.
Causes
The cause of achalasia is unknown. Theories on causation invoke infection, heredity or an abnormality of the immune system that causes the body itself to damage the esophagus (autoimmune disease).
The esophagus contains both muscles and nerves. The nerves coordinate the relaxation and opening of the sphincters as well as the peristaltic waves in the body of the esophagus. Achalasia has effects on both the muscles and nerves of the esophagus; however, the effects on the nerves are believed to be the most important. Early in achalasia, inflammation can be seen (when examined under the microscope) in the muscle of the lower esophagus, especially around the nerves. As the disease progresses, the nerves begin to degenerate and ultimately disappear, particularly the nerves that cause the lower esophageal sphincter to relax. Still later in the progression of the disease, muscle cells begin to degenerate, possibly because of the damage to the nerves. The result of these changes is a lower sphincter that cannot relax and muscle in the lower esophageal body that cannot support peristaltic waves. With time, the body of the esophagus stretches and becomes enlarged (dilated).
Symptoms
The most common symptom of achalasia is difficulty in swallowing (dysphagia). Patients typically describe food sticking in the chest after it is swallowed. Dysphagia occurs with both solid and liquid food. Moreover, the dysphagia is consistent, meaning that it occurs during virtually every meal.
Sometimes, patients will describe a heavy sensation in their chest after eating that may force them to stop eating. Occasionally, pain may be severe and mimic heart pain (angina). The cause of this discomfort is felt to be the accumulation of ingested food within the esophagus.
Regurgitation of food that is trapped in the esophagus can occur, especially when the esophagus is dilated. If the regurgitation happens at night while the patient is sleeping, food can enter the throat and cause coughing and choking. If the food enters the trachea (windpipe) and lung, it can lead to infection (aspiration pneumonia).
Because of the problem with swallowing food, a large proportion of patients with achalasia lose weight. Episodes of chest pain may also occur especially with vigorous achalasia. Sometimes symptoms suggest gastroesophageal reflux disease (GERD); however, it's not clear if the symptoms are, in fact, due to reflux. Moreover, acid suppression rarely improves the symptoms of achalasia.
Treatment
Treatments for achalasia include oral medications, stretching of the lower esophageal sphincter (dilation), surgery to cut the sphincter (esophagomyotomy), and the injection of botulinum toxin (Botox) into the sphincter. All four treatments reduce the pressure within the lower esophageal sphincter to allow easier passage of food from the esophagus into the stomach.
Oral medications
Oral medications that help to relax the lower esophageal sphincter include groups of drugs called nitrates, for example, isosorbide dinitrate (Isordil) and calcium channel blockers, for example, nifedipine (Procardia) and verapamil (Calan). Although some patients with achalasia, particularly early in the disease, have improvement of symptoms with medications, most do not. By themselves, oral medications are likely to provide only short-term and not long-term relief of the symptoms of achalasia, and many patients experience side-effects from the medications.
Dilation
The lower esophageal sphincter also may be treated directly by forceful dilation. Dilation of the lower esophageal sphincter is done by having the patient swallow a tube with a balloon at the end. The balloon is placed across the lower sphincter with the help of X-rays, and the balloon is blown up suddenly. The goal is to stretch--actually to tear--the sphincter. The success of forceful dilation has been reported to be between 60% and 95%. Patients in whom dilation is not successful can undergo further dilations, but the rate of success decreases with each additional dilation. If dilation is not successful, the sphincter may still be treated surgically. The main complication of forceful dilation is rupture of the esophagus, which occurs 5% of the time. Half of the ruptures heal without surgery, though patients with rupture who do not require surgery should be followed closely and treated with antibiotics. The other half of ruptures require surgery. (Although surgery carries additional risk for the patient, surgery can repair the rupture as well as permanently treat the achalasia with esophagomyotomy.) Death following forceful dilation is rare. Dilation is a quick and inexpensive procedure compared with surgery, and requires only a short hospital stay.
Esophagomyotomy
The sphincter also can be cut surgically, a procedure called esophagomyotomy. The surgery can be done using an abdominal incision or laparoscopically through small punctures in the abdomen. In general, the laparoscopic approach is used with uncomplicated achalasia. Alternatively, the surgery can be done with a large incision or laparoscopically through the chest. Esophagomyotomy is more successful than forceful dilation, probably because the pressure in the lower sphincter is reduced to a greater extent and more reliably; 80%-90% of patients have good results. With prolonged follow-up, however, some patients develop recurrent dysphagia. Thus, esophagomyotomy does not guarantee a permanent cure. The most important side effect from the more reliable and greater reduction in pressure with esophagomyotomy, is reflux of acid (gastroesophageal reflux disease or GERD). In order to prevent this, the esophagomyotomy can be modified so that it doesn't completely cut the sphincter or the esophagomyotomy may be combined with anti-reflux surgery (fundoplication). Whichever surgical procedure is done, some physicians recommend life-long treatment with oral medications for acid reflux. Others recommend 24 hour esophageal acid testing with lifelong medication only if acid reflux is found.
I find something in herbal medicine good to share on here with anyone suffering from the disease such as HIV, Herpes, Hepatitis or Chronic Lyme Disease,Parkinson's disease,Schizophrenia,Lung Cancer,Breast Cancer,Colo-Rectal Cancer,Blood Cancer,Prostate Cancer,siva.Fatal Familial Insomnia Factor V Leiden Mutation ,Epilepsy Dupuytren's disease,Desmoplastic small-round-cell tumor Diabetes ,Coeliac disease,Creutzfeldt–Jakob disease,Cerebral Amyloid Angiopathy, Ataxia,Arthritis,Amyotrophic Lateral Scoliosis,Fibromyalgia,Fluoroquinolone ToxicitySyndrome Fibrodysplasia Ossificans ProgresSclerosis,Seizures,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic diseases.Hiv_ Aids,Herpe ,Copd,Glaucoma., Cataracts,Macular degeneration,Cardiovascular disease,Lung disease.Enlarged prostate,Osteoporosis.Alzheimer's disease,
ReplyDeleteDementia.
Lupus as well.Dr Itua herbal made cure my HIV and gave me hope that he can cure all types of diseases I believed him) I do the best of myself that I can do, I went for a program in west Africa about fashion on another side I was HIV positive. I walk through a nearby village for our program schedule then I found a signage notice that says Dr Itua Herbal Center then I asked my colleagues what all about this very man called Dr Itua, She told me that he's a herbal doctor and he can cure all kind of disease i walked to him and explain myself to him as I'm a strangler out there he prepared me herbal medicine and told me how to drink it for two weeks, when I get to my hotel room I take a look at it then says a prayer before I drank it not knowing after two weeks I went to test and I found out I was negative I ran to him to pay him more but he refuses and says I should share his works for me around the globe so sick people can see as well. I'm writing a lot about him this season so that is how I was cured by drinking Dr Itua herbal medicine, He's A caring man with godly heart. Well - everything I decided all go through for me well and how you're going to treat this new aspect to your life. You don't have to suffer alone, and it's okay to ask for help. It also doesn't have to be a constant demon, as you'll get to know your body and yourself in a much deeper way than most people. Take advantage of this, as it will help you appreciate Africa Herbal Made.
Dr Itua Contact Information.
Email...drituaherbalcenter@gmail.comWhatsapp Number....+2348149277967